Nursing Care Plan for Fistula: Promoting Healing and Optimizing Quality of Life
Introduction:
A fistula is an abnormal connection between two body structures, often resulting from trauma, infection, or surgery. Fistulas can cause significant physical discomfort and may require ongoing management and support. As a nurse, your role is crucial in assessing and addressing the needs of individuals with fistulas. This nursing care plan aims to outline evidence-based interventions to assess, manage, and support patients with a fistula.
Patient Assessment For Fistula:
- Name: [Patient’s Name]
- Age: [Patient’s Age]
- Gender: [Patient’s Gender]
- Medical History: [Brief summary of patient’s medical history]
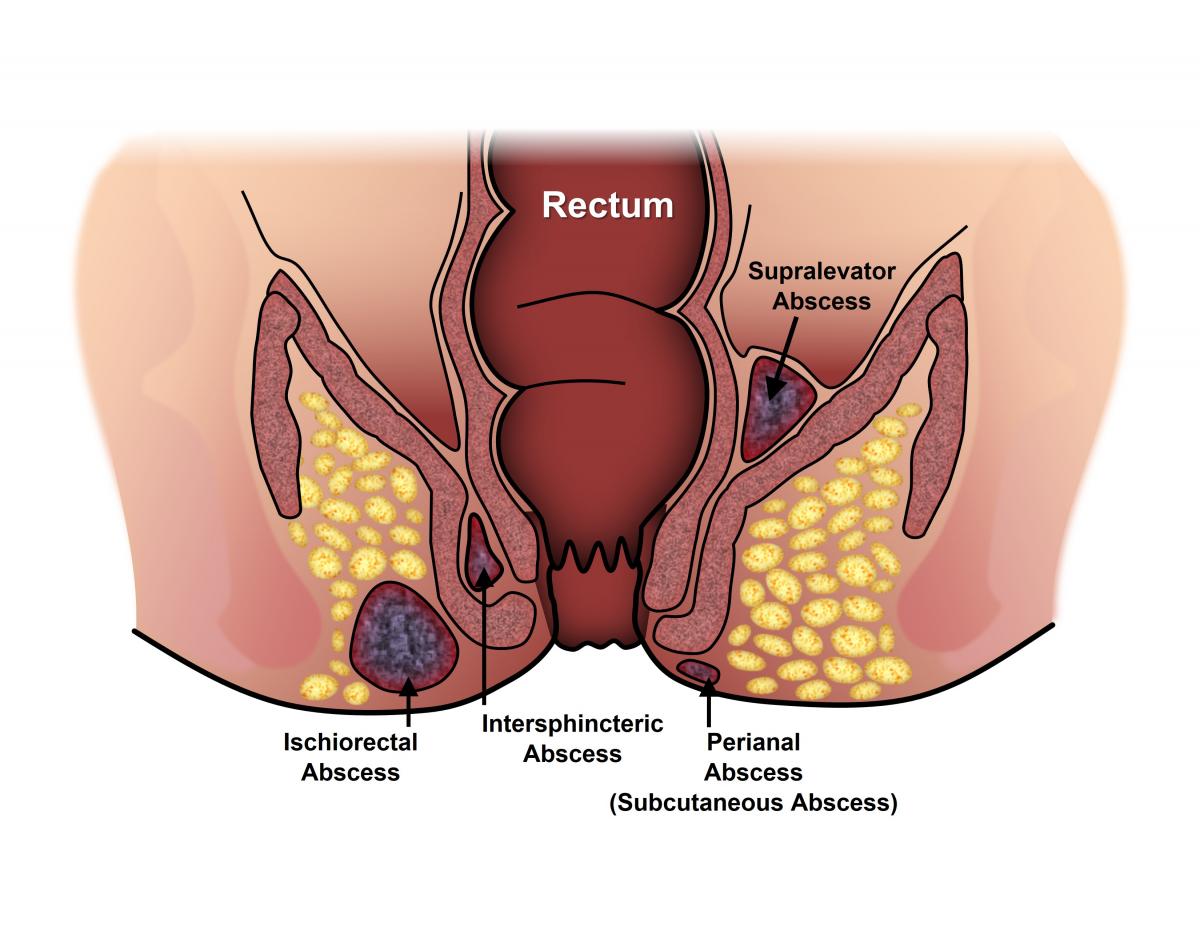
- Type of Fistula: [Identify the location and type of fistula]
- Underlying Cause: [Identify the underlying cause of the fistula]
Comprehensive Patient Assessment:
- Gather a detailed medical history, including the cause, location, and duration of the fistula.
- Assess the characteristics of the fistula, such as size, location, and amount of fluid leakage.
- Evaluate the patient’s overall physical health, nutritional status, and presence of comorbidities.
- Consider the patient’s emotional well-being, coping strategies, and the impact of the fistula on their daily life.
Wound Assessment:
- Examine the fistula site for signs of infection, inflammation, or poor wound healing.
- Monitor the amount, color, and consistency of the fluid leakage from the fistula.
- Assess the surrounding skin for irritation, maceration, or breakdown.
Nursing Diagnosis of Fistula:
- Impaired Tissue Integrity related to the presence of the fistula and potential for infection.
- Risk for Imbalanced Nutrition: Less than Body Requirements related to altered digestion and absorption.
- Disturbed Body Image related to the presence of a visible fistula and associated odor or drainage.
- Deficient Knowledge regarding fistula management, self-care, and prevention of complications.
- Impaired Skin Integrity related to fistula leakage and potential skin breakdown.
- Risk for Infection related to the presence of an open wound and exposure to microorganisms.
- Disturbed Body Image related to the presence of a visible fistula and changes in appearance.
- Anxiety related to the physical and emotional impact of living with a fistula.
Nursing Interventions and Planning:
Impaired Tissue Integrity:
- Assess the fistula site regularly for signs of infection, such as redness, swelling, warmth, or purulent drainage.
- Implement appropriate wound care techniques, such as cleansing with sterile solutions, applying sterile dressings, and promoting a moist healing environment.
- Collaborate with the healthcare team to determine the need for antibiotic therapy or other interventions to prevent or treat an infection.
- Educate the patient and caregivers about the signs of infection, proper wound care techniques, and the importance of reporting any changes promptly.
Risk for Imbalanced Nutrition: Less than Body Requirements:
- Assess the patient’s nutritional status, including weight, dietary intake, and signs of malnutrition.
- Collaborate with the healthcare team to develop a nutrition plan that meets the patient’s specific needs, which may include a high-calorie, high-protein diet or nutritional supplements.
- Provide education on dietary modifications, such as avoiding foods that exacerbate symptoms or worsen fistula output.
- Monitor the patient’s nutritional status regularly and adjust the plan as necessary based on their response and changing needs.
Disturbed Body Image:
- Assess the patient’s feelings and concerns regarding the presence of the fistula, including any associated odor or drainage.
- Provide emotional support and create a non-judgmental environment for the patient to express their emotions and body image concerns.
- Assist the patient in developing coping strategies, such as counseling or support groups, to address body image issues and enhance self-esteem.
- Educate the patient and caregivers about strategies to manage odor or drainage, such as the use of odor-absorbing dressings or pouches.
Deficient Knowledge:
- Assess the patient’s understanding of the fistula, its causes, and potential complications.
- Provide education on fistula management, including proper hygiene, wound care techniques, and prevention of complications.
- Teach the patient and caregivers about signs of infection, when to seek medical attention and potential dietary modifications.
- Offer written materials or resources for the patient and caregivers to refer to for additional information and support.
Wound Care and Hygiene:
- Cleanse the fistula site using gentle, non-irritating solutions and a sterile technique.
- Apply appropriate dressings, such as non-adherent dressings or absorbent pads, to absorb the fluid leakage and protect the surrounding skin.
- Implement strategies to promote wound healing, such as optimizing nutrition, maintaining adequate hydration, and promoting rest.
Infection Prevention:
- Promote meticulous hand hygiene for both the patient and healthcare providers.
- Educate the patient on proper wound care techniques, including cleaning and dressing changes, to minimize the risk of infection.
- Administer prophylactic antibiotics, as prescribed, to prevent or treat infection.
Psychosocial Support:
- Provide emotional support and reassurance to the patient, addressing their concerns and fears related to living with a fistula.
- Encourage the patient to express their feelings and offer counseling or referral to a mental health professional if needed.
- Facilitate support groups or connect the patient with others living with fistulas to foster a sense of community and understanding.
Nutritional Support:
- Collaborate with a registered dietitian to develop an individualized nutrition plan that supports wound healing and overall health.
- Ensure the patient receives adequate protein, vitamins, and minerals to optimize tissue repair and prevent malnutrition.
- Educate the patient on the importance of a balanced diet and the role of nutrition in wound healing.
Education and Self-Management:
- Educate the patient on self-care strategies, including proper hygiene, wound monitoring, and signs of infection to report.
- Teach the patient techniques for managing and concealing the fistula, such as the use of specialized clothing or absorbent pads.
- Provide information on available resources, such as support groups, online communities, and educational materials about fistulas.
Evaluation and Expected Outcomes:
- Improved tissue integrity with the prevention or treatment of infection.
- Achievement of balanced nutrition and prevention of malnutrition-related complications.
- Enhanced body image and improved coping strategies to address concerns related to the fistula.
- Increased knowledge and understanding of fistula management, self-care, and prevention of complications.
Documentation: Regularly document the assessment findings, interventions provided, and the patient’s response to treatment. Collaborate with the interdisciplinary healthcare team to review and update the care plan based on the patient’s condition and evolving needs.
Note: This nursing care plan is a general guideline and should be individualized based on the patient’s specific needs, type of fistula, and healthcare provider’s recommendations.

3 Responses
Very useful nursing care plan and applicable
Very useful nursing care plan
Nice nursing care plan and applicable