Nursing Care Plan for Dengue Fever
Introduction:
Dengue fever is a mosquito-borne viral infection that can cause a range of symptoms, from mild flu-like symptoms to severe dengue hemorrhagic fever. As a nurse, your role is crucial in providing supportive care, monitoring for complications, and promoting the well-being of individuals with dengue fever. This nursing care plan aims to outline evidence-based interventions to assess, manage, and support patients with dengue fever.
A nursing care plan for dengue fever focuses on managing symptoms, preventing complications, and supporting recovery from this mosquito-borne viral infection. Dengue fever is caused by the dengue virus, transmitted by Aedes mosquitoes, and is commonly found in tropical and subtropical regions. Patients with dengue fever often experience high fever, severe headache, joint and muscle pain, rash, and, in severe cases, hemorrhagic symptoms or dengue shock syndrome. Due to the potential for rapid progression and serious complications, timely and comprehensive nursing care is essential.
The care plan emphasizes close monitoring of vital signs, hydration management, and pain relief to support the patient’s comfort and well-being. Additionally, education on preventing mosquito bites and recognizing warning signs of severe dengue is crucial to prevent spread and ensure early intervention. This nursing care plan aims to provide targeted interventions that support the patient’s immune response, manage symptoms, and mitigate risks, ultimately promoting a safe recovery.
Patient Information:
- Name: [Patient’s Name]
- Age: [Patient’s Age]
- Gender: [Patient’s Gender]
- Medical History: [Brief summary of patient’s medical history]
- Type of Dengue: [Note if it is dengue fever or dengue hemorrhagic fever]
- Symptoms: [Describe the patient’s presenting symptoms, such as fever, headache, rash, joint pain, etc.]
- Medical Diagnosis: Dengue
- Fever Admission Date: [Admission Date]
- Care Plan Initiated: [Care Plan Initiation Date]
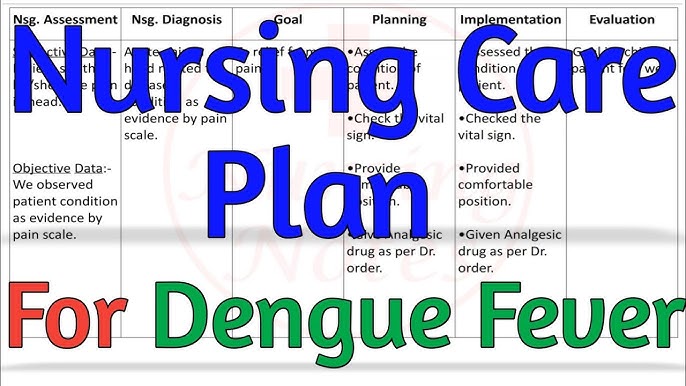
Nursing Assessment:
A thorough nursing assessment for a patient with dengue fever is essential for identifying symptoms, monitoring progression, and implementing appropriate interventions to manage the illness effectively. Key components of the assessment include:
Subjective Data:
- The patient complained of severe headache, joint and muscle pain, and high fever.
- The patient reports feeling fatigued and weak.
- The patient may express anxiety or distress due to the symptoms.
Objective Data:
- Elevated body temperature (above 38°C/100.4°F).
- Presence of rash on the body.
- Positive tourniquet test.
- Decreased platelet count (below 150,000/mm3).
- Signs of dehydration (e.g., dry mucous membranes, decreased urine output, increased heart rate).
1. Vital Signs
- Temperature: Monitor for high fever, often above 102°F (39°C), as fever is one of the main symptoms of dengue.
- Blood Pressure: Assess for any signs of hypotension, as it can indicate progression toward severe dengue or shock.
- Heart Rate: Check for tachycardia, which can be present due to fever or dehydration.
2. Hydration Status
- Fluid Intake and Output: Record daily intake and output to monitor hydration, as patients with dengue are at high risk of dehydration due to fever and reduced oral intake.
- Skin Turgor and Mucous Membranes: Assess for dry mucous membranes, sunken eyes, and decreased skin turgor, which are signs of dehydration.
- Weight: Daily weight measurements can help detect fluid loss or retention, providing an indicator of hydration status.
3. Pain Assessment
- Headache and Muscle Pain: Ask about the severity and location of pain, as dengue often causes intense headaches and body aches.
- Joint Pain: Document joint pain or “breakbone fever” pain, a characteristic symptom of dengue that can significantly impact comfort.
- Abdominal Pain: Monitor for abdominal pain, which can be an early sign of progression to severe dengue.
4. Bleeding and Hemorrhagic Signs
- Skin and Mucous Membranes: Assess for petechiae, bruising, or bleeding gums, as these can indicate a drop in platelet count or hemorrhagic manifestations.
- Stool and Urine: Monitor for any blood in stool or urine, as this could signal internal bleeding.
- Nasal or Gum Bleeding: Check for any minor bleeding episodes, which may indicate the need for urgent platelet monitoring and intervention.
5. Skin Assessment
- Rash: Observe for a characteristic dengue rash, which may appear on the chest, back, or limbs. Document any progression or spread of the rash.
- Skin Warmth: The skin may feel warm due to high fever; monitor for changes that could indicate the onset of fever or cooling after the fever subsides.
6. Neurological Assessment
- Mental Status: Evaluate for any confusion, irritability, or restlessness, which may indicate hypoperfusion or complications from the disease.
- Level of Consciousness: Assess for any changes in consciousness, especially if dengue progresses to severe stages where shock or complications might impact mental status.
7. Laboratory Values
- Platelet Count: Regularly review lab results for platelet counts, as a significant drop is common in dengue and can increase the risk of bleeding.
- Hematocrit: Monitor hematocrit levels to assess for hemoconcentration, which may indicate dehydration or an increased risk of dengue hemorrhagic fever.
- Liver Enzymes: Elevated liver enzymes may be present in dengue cases, indicating liver involvement and the need for additional care.
This comprehensive nursing assessment provides a foundation for developing a care plan that addresses the patient’s hydration, pain management, and monitoring for potential complications. Regular assessments allow for timely interventions, supporting recovery and preventing the progression of severe symptoms.
Nursing Diagnosis:
Based on the assessment findings for a patient with dengue fever, here are potential nursing diagnoses to address the patient’s specific needs and risks:
1. Hyperthermia Related to Viral Infection
- Evidence: Elevated body temperature (fever above 102°F), flushed skin, sweating.
- Goal: Reduce fever to within normal range and improve comfort.
2. Risk for Deficient Fluid Volume Related to Fever and Reduced Oral Intake
- Evidence: Signs of dehydration such as dry mucous membranes, decreased skin turgor, and reduced urine output.
- Goal: Maintain adequate hydration and prevent complications associated with fluid imbalance.
3. Acute Pain Related to Headache, Muscle Aches, and Joint Pain
- Evidence: The patient reports of severe headache, joint pain, and muscle aches (commonly described as “breakbone fever”).
- Goal: Decrease pain levels to improve comfort and promote rest.
4. Risk for Bleeding Related to Thrombocytopenia (Low Platelet Count) and Hemorrhagic Tendency
- Evidence: Low platelet count, presence of petechiae, gum bleeding, or other signs of spontaneous bleeding.
- Goal: Prevent bleeding episodes and monitor for early signs of hemorrhagic complications.
5. Risk for Impaired Skin Integrity Related to Rash and Pruritus (Itching)
- Evidence: Presence of dengue rash, potential for itching that may lead to skin breakdown if scratched.
- Goal: Maintain skin integrity by minimizing itching and preventing skin breakdown.
6. Risk for Ineffective Tissue Perfusion Related to Potential Complications (e.g., Hemorrhagic Shock)
- Evidence: Low blood pressure, tachycardia, potential for progression to severe dengue or dengue shock syndrome.
- Goal: Ensure adequate tissue perfusion and monitor for signs of shock or decreased perfusion.
7. Fatigue Related to Fever, Pain, and Generalized Weakness
- Evidence: Patient reports feeling weak, tired, and lacking energy, with decreased ability to participate in activities.
- Goal: Improve energy levels by managing symptoms and promoting rest and recovery.
8. Knowledge Deficit Related to Disease Process and Preventive Measures
- Evidence: Patient and/or family show limited understanding of dengue fever, symptom management, and prevention of mosquito bites.
- Goal: Increase knowledge about dengue fever, including symptoms to monitor, necessary precautions, and prevention strategies.
These nursing diagnoses provide a structured approach for managing the patient’s symptoms, preventing complications, and educating both the patient and family. They guide the nursing interventions needed to support recovery and ensure patient safety throughout the course of the illness.
Nursing Interventions and Rationales:
Risk for Fluid Volume Deficit:
- Monitor vital signs, intake, and output closely to assess fluid balance.
- Encourage oral fluid intake unless contraindicated by vomiting or altered mental status.
- Administer intravenous fluids as prescribed to maintain adequate hydration and prevent hypovolemia.
- Assess for signs of fluid overload or impending shock, such as respiratory distress or hypotension, and promptly report to the healthcare team.
Risk for Infection:
- Practice strict hand hygiene and adhere to infection prevention protocols.
- Implement measures to prevent mosquito bites, such as using mosquito nets, wearing protective clothing, and applying insect repellent.
- Educate the patient and caregivers about the importance of avoiding stagnant water and maintaining a clean environment to prevent mosquito breeding.
- Monitor for signs of secondary infections, such as fever, increased respiratory rate, or localized signs of infection, and promptly report to the healthcare team.
Risk for Bleeding:
- Monitor the patient’s platelet count regularly.
- Implement bleeding precautions, such as using a soft toothbrush, avoiding invasive procedures, and minimizing the use of venipuncture.
- Apply pressure to injection sites for an appropriate duration after injections.
- Monitor for signs of bleeding, such as petechiae, ecchymosis, or hematuria.
- Report any abnormal bleeding immediately to the healthcare provider.
Acute Pain:
- Assess the patient’s pain level and characteristics regularly.
- Administer prescribed pain medications as appropriate, ensuring timely administration and monitoring for side effects.
- Apply cold compresses or provide comfort measures, such as relaxation techniques or distraction, to alleviate pain.
- Collaborate with the healthcare team to address any underlying causes of pain, such as abdominal complications or severe joint pain.
Knowledge Deficit:
- Assess the patient’s understanding of dengue fever, its transmission, and preventive measures.
- Provide education about dengue fever, including symptoms, complications, and when to seek medical attention.
- Teach the patient and caregivers about measures to prevent mosquito bites and reduce the risk of dengue fever transmission.
- Discuss the importance of follow-up appointments and monitoring for potential complications, such as dengue hemorrhagic fever.
Nursing Goals:
- The patient will experience relief from discomfort within [timeframe].
- The patient will maintain adequate fluid volume as evidenced by stable vital signs, improved urine output, and moist mucous membranes.
- The patient will demonstrate reduced anxiety by expressing decreased restlessness and increased participation in self-care activities.
- The patient will maintain hemostasis and prevent bleeding complications.
- The patient will demonstrate an understanding of dengue fever prevention measures and self-care management before discharge.
Evaluation and Expected Outcomes:
- Maintenance of fluid balance with adequate hydration and prevention of hypovolemia.
- Prevention of secondary infections through infection control measures and vigilant monitoring.
- Alleviation of acute pain through appropriate pain management interventions.
- Improved knowledge and understanding of dengue fever management, complications, and preventive measures.
- The patient reports a reduction in discomfort within the specified timeframe.
- Vital signs indicate stable fluid balance, improved urine output, and moist mucous membranes.
- The patient demonstrates decreased restlessness and increased participation in self-care activities.
- The patient maintains hemostasis without any bleeding complications.
- The patient exhibits an understanding of dengue fever prevention measures and self-care management during the discharge teaching session.
Documentation: Regularly document the patient’s vital signs, fluid balance, pain assessments, interventions provided, and the patient’s response to treatment. Collaborate with the interdisciplinary healthcare team to review and update the care plan based on the patient’s condition and evolving needs.
Note: This care plan is a general guideline. Actual interventions and goals may vary depending on the patient’s condition, medical orders, and individualized assessment. It is important to consult with the healthcare team and adapt the care plan accordingly.

One Response
Goox