Nursing Care Plan for Gastrointestinal (GI) Bleed
Introduction:
Gastrointestinal (GI) bleeding refers to the loss of blood from the digestive tract, which can occur in various areas such as the esophagus, stomach, or intestines. As a nurse, your role is crucial in the assessment, management, and support of patients experiencing GI bleeding. This nursing care plan aims to outline evidence-based interventions to assess, manage, and support patients with GI bleeding.
Patient Information:
- Name: [Patient’s Name]
- Age: [Patient’s Age]
- Gender: [Patient’s Gender]
- Medical Diagnosis: Gastrointestinal Bleed
- Date of Admission: [Date]
- Allergies: [Patient’s Known Allergies]
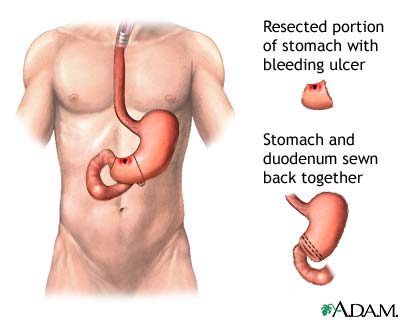
- Underlying Cause of GI Bleed: [Identify the underlying cause, such as peptic ulcer disease, gastritis, or diverticulosis]
- Date of Admission: [Date of Admission]
- Date of Care Plan: [Date of Care Plan]
Nursing Assessment For GI Bleed:
Subjective Data:
- Patients may report symptoms such as abdominal pain, nausea, vomiting, or passage of dark, tarry stools.
- Patients may express concerns about the cause of the bleeding and potential complications.
Objective Data:
- Documentation of signs of bleeding, such as hematemesis (vomiting blood) or melena (dark, tarry stools).
- Physical examination findings may include pallor, hypotension, tachycardia, and signs of hypovolemia.
- Laboratory results may indicate a decrease in hemoglobin and hematocrit levels.
Vital Signs:
- Blood Pressure: [Patient’s BP]
- Heart Rate: [Patient’s HR]
- Respiratory Rate: [Patient’s RR]
- Temperature: [Patient’s Temperature]
General Appearance:
- Pale skin
- Fatigue
- Dizziness
Gastrointestinal Assessment:
- Abdominal pain
- Hematemesis (vomiting blood)
- Melena (black, tarry stools)
- Hematochezia (bright red blood in stool)
- Decreased bowel sounds
Laboratory Tests:
- Hemoglobin and Hematocrit levels
- Coagulation profile
- Liver function tests
- Electrolyte levels
- Blood type and cross-match
Nursing Diagnosis For GI Bleed:
- Ineffective Tissue Perfusion related to blood loss secondary to GI bleed.
- Risk for Deficient Fluid Volume related to excessive bleeding.
- Acute Pain related to abdominal discomfort and tissue ischemia.
- Imbalanced Nutrition: Less Than Body Requirements related to decreased oral intake and blood loss.
- Anxiety related to health conditions and hospitalization.
- Acute Pain related to GI bleeding and associated abdominal discomfort as evidenced by the patient’s report of abdominal pain.
- Risk for Deficient Fluid Volume related to blood loss and inadequate fluid replacement as evidenced by signs of hypovolemia, such as pallor and hypotension.
- Anxiety related to the uncertainty of the bleeding cause and potential complications as evidenced by the patient’s expressions of worry, restlessness, or fear.
Nursing Interventions:
Ineffective Tissue Perfusion:
- Monitor vital signs frequently to assess for changes in blood pressure, heart rate, and oxygen saturation.
- Administer supplemental oxygen as prescribed to improve oxygenation.
- Elevate the head of the bed to promote venous return and improve tissue perfusion.
- Administer blood products (packed red blood cells, fresh frozen plasma) as prescribed to replace lost blood volume.
Risk for Deficient Fluid Volume:
- Monitor intake and output to assess fluid balance.
- Administer intravenous fluids (isotonic solutions) as prescribed to maintain adequate hydration.
- Monitor laboratory values, including hemoglobin and hematocrit, to assess the effectiveness of fluid replacement therapy.
- Educate the patient on the importance of increasing oral fluid intake once the bleeding is controlled.
- Monitor and record vital signs, including blood pressure, heart rate, and oxygen saturation, to assess the patient’s hemodynamic status.
- Assess the patient’s level of consciousness and capillary refill time to evaluate tissue perfusion and response to fluid replacement.
- Administer intravenous fluids and blood products as ordered to restore and maintain fluid volume.
- Monitor intake and output to evaluate fluid balance and provide accurate fluid replacement therapy.
- Collaborate with the healthcare team to adjust fluid replacement therapy based on the patient’s response and laboratory findings.
Acute Pain:
- Assess the patient’s pain level using a pain scale and document the findings.
- Administer prescribed pain medications promptly to alleviate discomfort.
- Encourage the patient to adopt a comfortable position to reduce abdominal pain.
- Apply heat packs or cold packs to the abdomen, as appropriate, to provide pain relief.
Imbalanced Nutrition: Less Than Body Requirements:
- Collaborate with the dietitian to provide a well-balanced diet that meets the patient’s nutritional needs.
- Offer small, frequent meals to promote adequate oral intake.
- Provide nutritional supplements, such as high-protein drinks, if the patient has difficulty meeting nutritional requirements orally.
- Monitor the patient’s weight regularly to assess nutritional status.
Anxiety:
- Establish a therapeutic relationship with the patient, providing emotional support and reassurance.
- Teach relaxation techniques, such as deep breathing exercises, to help the patient manage anxiety.
- Encourage the patient to express concerns and provide appropriate information and education.
- Involve the patient’s family or support system in providing emotional support.
- Create a calm and reassuring environment for the patient.
- Encourage the patient to express their feelings and concerns about the GI bleed, treatment, and potential complications.
- Provide clear and accurate information about the cause of the bleeding, diagnostic tests, and treatment options.
- Educate the patient about the importance of rest and stress reduction techniques to support overall well-being.
- Refer the patient to counseling services or support groups to address their emotional needs and provide coping strategies.
Nursing Evaluation For GI Bleed:
- The patient’s vital signs stabilize within normal limits.
- Hemoglobin and hematocrit levels improve.
- The patient reports pain relief and demonstrates a decrease in pain scores.
- The patient demonstrates increased oral intake and adequate nutrition.
- The patient’s anxiety decreases, and they express a better understanding of their condition.
- The patient experiences a reduction in abdominal pain and reports improved comfort.
- The patient’s fluid volume is restored and maintained within an acceptable range.
- The patient reports reduced anxiety levels and demonstrates coping mechanisms to manage emotional distress.
- The patient actively engages in self-care strategies and seeks appropriate support when needed.
Note: This nursing care plan is a general guideline. Individual care plans may vary depending on the patient’s specific condition and healthcare facility protocols. It is important to collaborate with the healthcare team and individualize the care plan based on the patient’s needs.
